Healthcare insurance can be complex, but understanding your coverage is crucial. This article clarifies the Fidelis Care Essential Plan, explaining its benefits, potential challenges, and how to navigate the system effectively. We'll address key concerns for both patients and providers, focusing on access to care and reimbursement rates.
Access to Care: Expanding Reach, Navigating Challenges
The Fidelis Care Essential Plan significantly expands healthcare access, a positive development. However, increased enrollment presents challenges. Higher patient volumes can lead to longer wait times for appointments at doctors' offices and hospitals. While increased patient numbers benefit healthcare providers financially, lower reimbursement rates from the plan can offset this and create financial strain. This is similar to a popular restaurant experiencing a surge in customers but with each customer paying less.
The Reimbursement Riddle: Understanding Provider Payments
Insurance plans reimburse healthcare providers (doctors, hospitals, etc.) for services rendered. The Fidelis Care Essential Plan often uses lower reimbursement rates than traditional plans. This means providers receive less payment for each service provided compared to patients with other insurance plans. This lower reimbursement, potentially leading to financial instability for some providers, is a crucial factor influencing healthcare access and quality.
Is this lower reimbursement rate sustainable for providers? This is a core question that requires ongoing investigation and discussion.
Provider Perspectives: Balancing Financial Viability and Patient Care
Lower reimbursement rates present a difficult choice for healthcare providers. While the increased patient volume may seem beneficial, the reduced payment per service could negatively impact their financial stability, particularly for those offering specialized care or operating in resource-constrained areas. Some providers may choose to limit the number of Essential Plan patients to maintain financial viability, potentially impacting access. Others may implement efficiency measures to offset the lower reimbursement. The financial reality directly influences their ability to provide care.
What This Means for You: Maximizing Your Plan Benefits
Understanding the dynamics of the Fidelis Care Essential Plan is critical for patients. Here's how to effectively utilize your coverage:
Verify Network Participation: Before scheduling appointments, confirm your doctor and hospital are in-network. Out-of-network care usually results in higher out-of-pocket expenses.
Open Communication: Proactively discuss your Essential Plan coverage with your healthcare provider to understand any potential impacts on services or wait times. Transparent communication leads to the best outcomes.
Proactive Scheduling: For specialized care, schedule appointments well in advance to mitigate potential wait times resulting from increased patient volume.
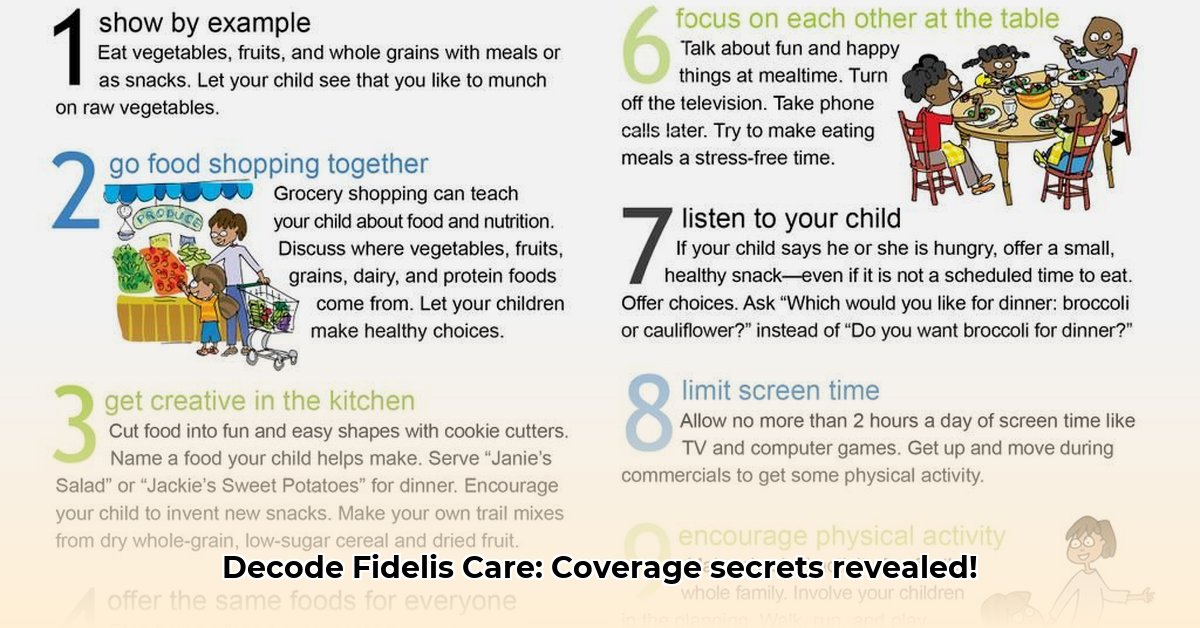
Prioritize Preventative Care: Use your plan's preventative care benefits (annual checkups, screenings), as this can help maintain health and potentially reduce costly future treatments.
The Bigger Picture: Collaboration for Sustainable Healthcare
Addressing the complexities of the Fidelis Care Essential Plan requires collective effort. Fidelis Care, healthcare providers, and policymakers need to work together to create a sustainable system. This includes exploring alternative reimbursement models and strategies to manage increased patient volume efficiently. The goal is a balanced healthcare system that ensures affordable access without jeopardizing the financial stability of healthcare providers. Ongoing collaboration and innovative solutions are critical to achieving this balance sustainably.
How Fidelis Essential Plan Reimbursement Impacts Rural Healthcare Provider Financial Stability
Rural healthcare providers face unique challenges. Lower reimbursement rates from plans like the Fidelis Essential Plan exacerbate these difficulties. Their smaller patient bases and often-limited resources make them particularly vulnerable to the financial implications of decreased reimbursement rates.
Understanding the Impact of Reimbursement Rates
The impact of reimbursement rates on rural clinics isn't uniform. Factors like the specific services offered and the patient demographic influence the effect. A clinic specializing in chronic care may experience a more significant financial strain than one focused on acute care. This disparity requires a nuanced understanding of its effects on various rural healthcare facilities.
Ripple Effects on Rural Healthcare Access
The financial strain from lower reimbursements can lead to:
- Service Reduction: Clinics may limit services or staff due to insufficient compensation.
- Reduced Access: Fewer providers and services mean less healthcare access for rural communities, disproportionately affecting vulnerable populations.
- Potential Closures: In severe cases, financial instability can lead to clinic closures, resulting in devastating healthcare access gaps for entire communities.
These consequences directly impact patients' health outcomes, potentially leading to worse health conditions through delayed or forgone care.
Advocating for Change: A Collaborative Approach
Addressing the financial challenges faced by rural providers requires comprehensive solutions:
- Transparency: Clarify reimbursement rates and their impact on rural healthcare.
- Negotiated Rates: Encourage collaboration between providers and insurers to negotiate fair reimbursement rates.
- Government Support: Explore policy changes and financial incentives to support rural healthcare providers.
- Innovative Models: Implement telehealth and other innovative care models to enhance efficiency and reduce costs.
- Patient Advocacy: Patients should advocate for policies that ensure access to quality care.
Sustaining rural healthcare requires collaborative efforts, focusing on both affordability and accessibility. Understanding reimbursement models is crucial in this endeavor.